Cancer immunotherapy has had many advances over the past decade. However there still is a great number of new options becoming available. These options present the opportunity for targeting individual patients and their specific lesions. We listed a new paper discussing these for prostate cancer, PCa. PCa is a complex cancer to treat for a variety of reasons. Many cases present as relatively indolent in nature whereas there is a small number which are highly aggressive. Understanding and identifying them is still a work in progress.
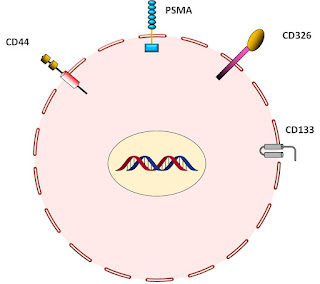
However we see options for doing so by using PCa cell surface markers. Using them we than have a variety of immunotherapeutic approaches.We show some of these below. Namely we look at stem cells, progression cells, and the tumor micro-environment. For the cell targets we look for surface markers. Then we can use antibodies, immune cells and even viral attacks. Our recent result considers the first two.
Consider a cancer cell with the surface markers as shown below. This is quite common for PCa cells, especially stem cells. We thus can look at the approaches below. First identify and find markers on the stem cells. The choose a CAR approach with one of several immune cells and/or choose an antibody approach using what are called poly specific antibodies.
Now antibodies, Ab, are common elements of the immune system.
As shown above they have a collection of proteins linked so that at the short end they attach to the target cell surface marker and at the lower end to an immune system cell. The result is elimination of the target. Think COVID. An example is below with an NK or natural killer cell. If a normal cell is found then it will have a surface marker MHC saying it is a good cell so do not do anything.
However if MHC is absent we get what we see below:
which results in an attack and elimination of the bad cell.
Thus we rely upon these Ab to help direct the immune cells to kill the bad or cancer cells. There are two possible ways to do this. One is to create Ab to attach to the cell and then wait for immune cells to attack. Or we can create immune cells with the ligand which can attach to the cancer cell. These are CAR or chimeric cells.
The malignant prostate cell typically has these 4 if not more targets as shown below.
Likewise the interaction between the NK cell and the PCa cell results from interactions as shown below.
Now the basic principle we espouse is that if we demand a set of multiple targets s shown above, not just one, then we get better targeting and less bad consequences. Namely we get to eliminate just what we want. We show that graphically below:
Now we can use what we call polyspecific Ab as shown below:
This is a 4th generation CAR. We have three ligand attachment areas plus when all 3 are attached they activate the release of cytokines and kill the cancer cell. These types of poly Ab are relatively easy to make and if they do the full attachment their have limited morbidity. They go after just the cancer cells and no others.
Now we can use Ab alone. Below we show a poly Ab attaching to a cell and then activating an immune cell.
These approaches are all based upon existing protocols. The demand the ability to identify the cancer cell and then produce the CAR or Ab as noted.
Production can be complex and costly as we show below for a CAR:
However CAR-T is more costly than CAR-NK. CAR-NK has shown to be readily produced with less side effects. The down side is the CAR-NK cells last only two weeks whereas the CAR-T for several months. But overall cost may be much lower. In contrast the poly Ab may be quite easy to produce in volume as shown with many of the Ab on the market today. In fact a library of them may be made readily available.
We believe that these techniques present great opportunities for change in dealing with this malignancy. However much of the above is still speculative depending on the results of clinical trials.